Presenters
- Lisa Tshuma, PA-C, DBH, MPAS, MPA, Assistant Professor, A.T. Still University, Mesa, AZ
- Valerie Sheridan, DO, FACOS, FACS, Assistant Dean of Clinical Education, A.T. Still University School of Osteopathic Medicine Arizona
Summary
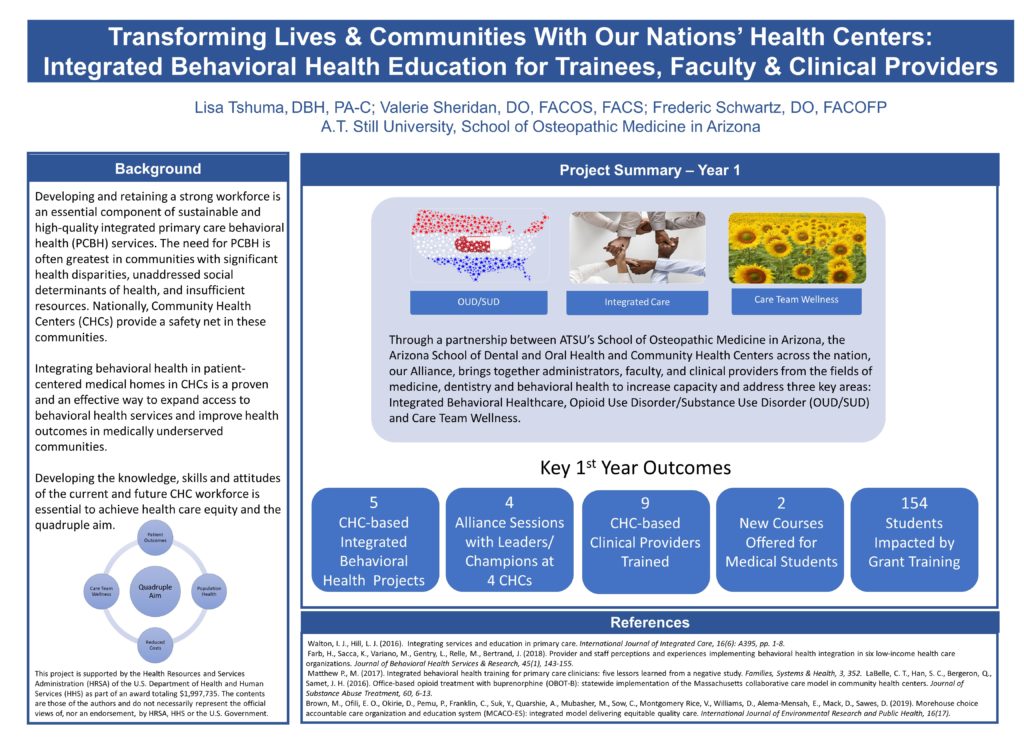
This poster describes an osteopathic medical school’s five-year education project partnering with several Community Health Centers (CHCs) across the nation. This project aims to advance integrated care, mitigate and treat opioid use disorder and substance use disorder (OUD/SUD), and improve patient, trainee and provider wellness within our partner clinics and communities. Developing and retaining the workforce is an essential component of sustainable and high-quality integrated primary care behavioral health (PCBH) services. However, the current literature is lacking in regards to best practices for teaching and evaluating primary care clinicians and training outcomes. The need for PCBH is often greatest in communities with significant health disparities, unaddressed social determinants of health, and insufficient resources. Nationally, CHCs provide a safety net in these communities. Integrating behavioral health in primary care medical homes in CHCs has proven to be an effective way to expand access to behavioral health services and improve health outcomes in medically underserved communities. Developing the knowledge and skills of the current and future CHC workforce is essential to achieve health care equity and the quadruple aim. In partnership with the National Association of Community Health Centers (NACHC), and with the support of a HRSA-PCTE grant, A.T. Still University (ATSU) is educating medical and dental trainees, as well as CHC providers through an innovative customized approach. The project is grounded by an alliance of medical educators and CHC-based administrative and clinical leaders who are not only transforming their own communities, but also sharing best practices with other CHC integrated care champions across the nation. The strategic design of this five-year project utilizes the development and implementation of integrated care projects at each CHC partner clinic, where students train for three years, as a longitudinal thread of learning. Through the ATSU Hometown Scholars program, students often hail from these same communities, facilitating a “dreamline” of students to service, bringing integrated care back to their own communities. In addition to integrated care being infused throughout their didactic curriculum, students have the opportunity to apply their integrated care knowledge and skills through CHC-based integrated care projects and elective coursework in the areas of OUD/SUD services, integrated behavioral health care delivery, and trainee and provider wellness. A key takeaway of this project is that patients, clinical providers, administrators, teachers and students are all subject to the same behavioral health risks. As COVID-19 has demonstrated, we are indeed, all in this together.
Objectives
- Identify the need for integrated behavioral health training in medical and dental curricula.
- Explain how increasing primary care provider and behavioral health clinician workforce capacity for integrated care contributes to equity in healthcare delivery.
- Describe the advantages of utilizing a customized, longitudinal interactive curricula to advance integrated care delivery and learning at community health centers.

Leave a Reply