Presenters
- Flora Ma, MS, Psychology Intern, Providence Medical Group, Newberg, OR
- Jeri Turgesen , PsyD, ABPP, MSCP, Board Certified Clinical Health Psychologist, Providence Medical Group – Newberg
- Jeremy Swindle, MD, Clinic Manager Family Medicine
- Kristin Tallman, PharmD, Clinical Pharmacist
- Ericka M Koellermeier, RN, Clinical Nurse
Summary
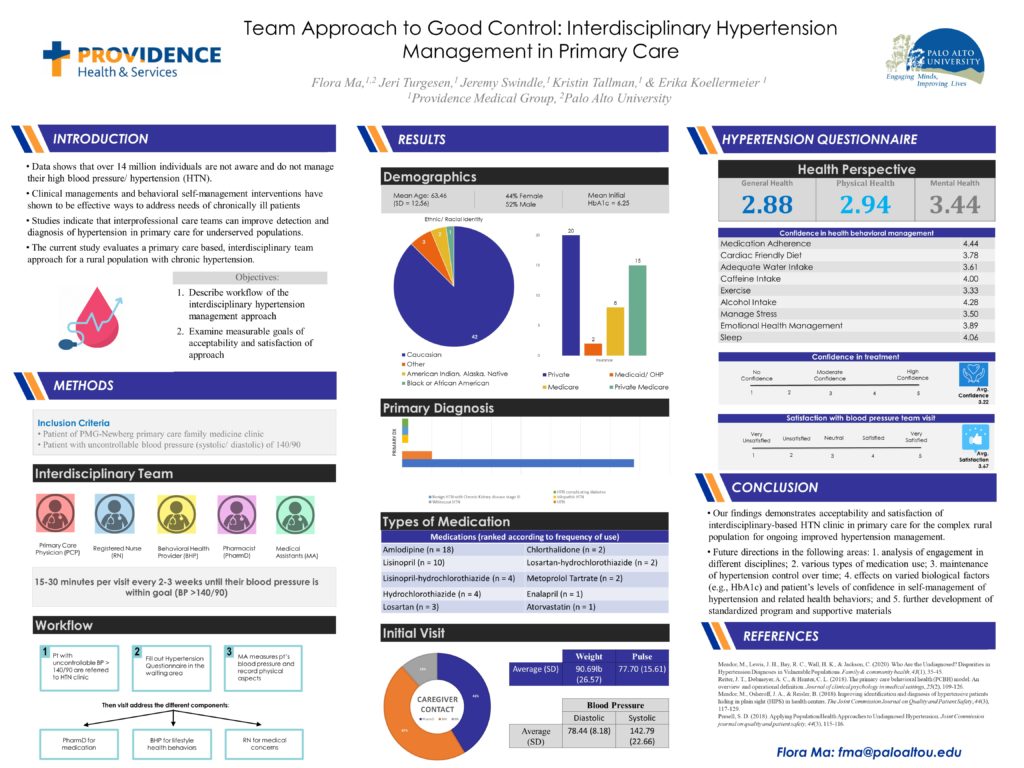
Recent data shows that over 14 million individuals are not aware of their hypertension and are not engaged in any interventions or taking any medications to control their blood pressure (Meador et al., 2020). Appropriate clinical and behavioral management, and competent self-management interventions have shown to be effective ways to address the physical and psychological needs of these chronically ill patients (Reiter, Dobmeyer, & Hunter, 2018). Research indicates that interprofessional care teams in addition to systematic analysis of electronic health record are strategies to improve detection and diagnosis of hypertension in primary care settings for underserved populations (Meador et al., 2018; Persell et al., 2018). The current interdisciplinary team care approach clinic program for a rural population with chronic hypertension describes the workflow process and measure feasibility to add to the existing knowledge of approaches to undiagnosed hypertension. This study analyzed historical data of patients who attended the hypertension clinic and have received multidisciplinary team-based approach in their hypertension appointments. Participants aged 18 years or older with blood pressure over 140/90 were referred by their primary care physician (PCP) to attend the hypertension clinic for appointments every 2-3 weeks until their blood pressure is within goal. Current evidence demonstrates the acceptability and satisfaction of the interdisciplinary-based hypertension clinic program in primary care for the rural population in Newberg, Oregon. Future directions include analysis of engagement in different disciplines, various types of medication use, effects on varied biological factors (e.g., Hba1c) and patient’s levels of confidence in self-management of different areas related to hypertension, and further development of program and supportive materials, such as standardized handouts about better management of hypertension.
Objectives
- Describe the workflow of the Interdisciplinary-based Hypertension Clinic Program in Primary Care and identify the role of each discipline.
- Define measurable goals of program acceptability and satisfaction
- Provide program evaluation materials and patient informational handouts to increase patient’s self-management of hypertension.

Leave a Reply