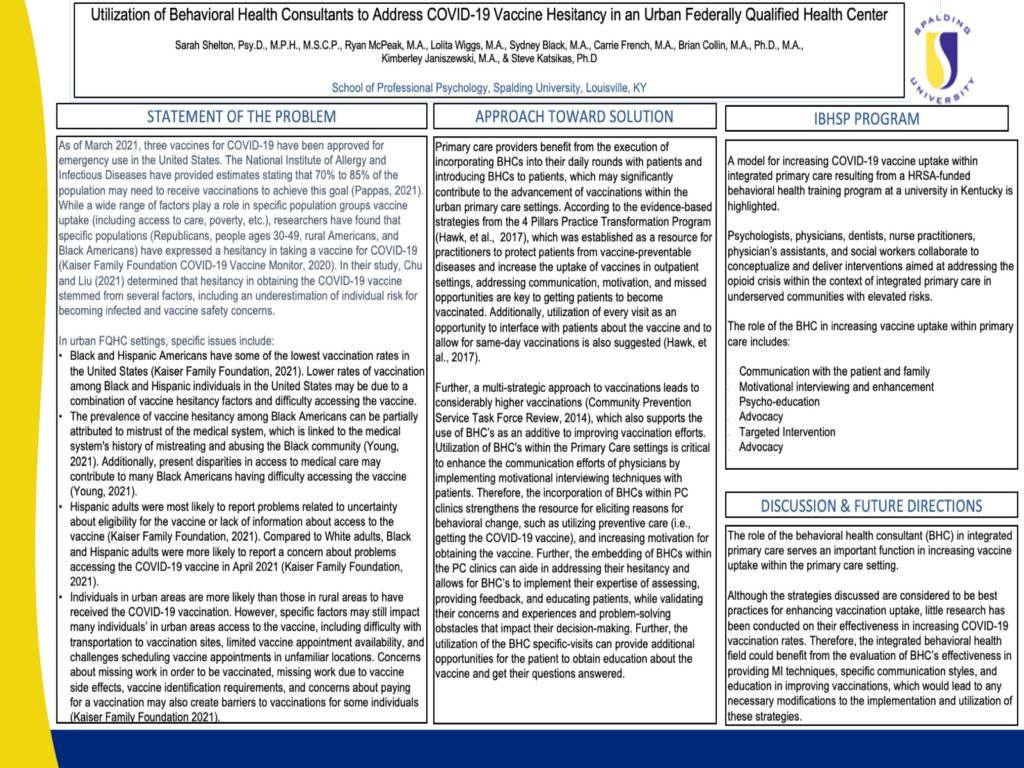
As of March 2021, three vaccines for COVID-19 have been approved for emergency use in the United States. While it is not clear exactly how many people need to be vaccinated in order to achieve the overall reduction in cases and lead to community immunity, the National Institute of Allergy and Infectious Diseases have provided estimates stating that 70% to 85% of the population may need to receive vaccinations to achieve this goal (Pappas, 2021). While a wide range of factors play a role in specific population groups vaccine uptake (including access to care, poverty, etc.), researchers have found that specific populations (Republicans, people ages 30-49, rural Americans, and Black Americans) have expressed a hesitancy in taking a vaccine for COVID-19 (Kaiser Family Foundation COVID-19 Vaccine Monitor, 2020). In their study, Chu and Liu (2021) determined that hesitancy in obtaining the COVID-19 vaccine stemmed from several factors, including an underestimation of individual risk for becoming infected and vaccine safety concerns. The authors also found that an understanding of positive community benefit and a realistic understanding of individual risks and benefits reduced hesitancy. In addressing vaccine hesitancy, Behavioral Health Consultants (BHCs) working in an integrated care model can play an essential role of facilitating the types of communication and counseling that serve to reduce vaccine hesitancy. This poster presents communication strategies best practices when providing communication and education to patients in an urban Federally Qualified Health Center serving a primary population consisting of people of color.
Spring Virtual Conference April 17-18th | In-Person Annual Conference in San Antonio, TX Oct 24-26th

Awesome work!!! Thank you for all that you are doing!!!