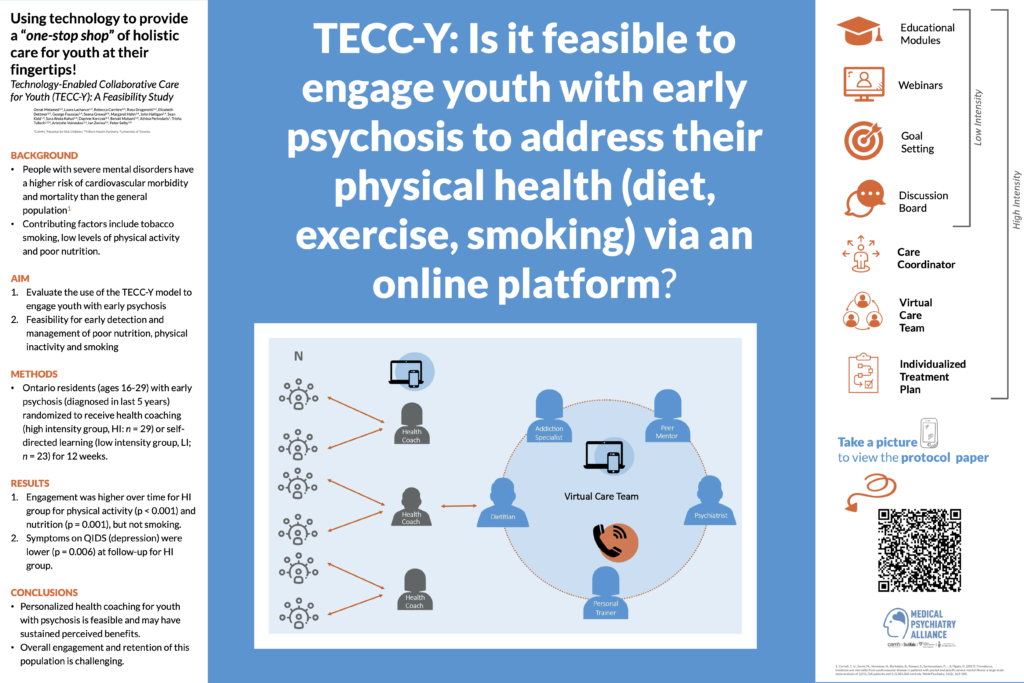
Objective: Psychotic disorders are associated with excess morbidity and premature mortality. Contributing factors include tobacco smoking, low levels of physical activity, and poor nutrition. Primary care for people with psychotic disorders is often fragmented and difficult to access. Digital interventions hold promise to facilitate integration of physical health care. Therefore, this study tested the feasibility and impact of a Technology-Enabled Collaborative Care for Youth (TECC-Y) model to improve health behaviors among youth with early psychosis. Methods: A feasibility study among youth (ages 16-29) with early psychosis (diagnosed in the past 5 years) in Ontario, Canada. Participants were randomly assigned to a health coach supervised by a virtual care team (VCT) (high intensity, HI; n=29), or a self-directed learning group (low intensity, LI; n=23) for 12 weeks. The primary outcome was client engagement, measured as self-perceived benefit of changing health behaviors. Exploratory outcomes included measures of health behaviors. Results: Engagement was higher for HI participants for physical activity (adjusted group difference in change at 24 weeks=3.4, CI95%=1.9-4.9, p<0.001) and nutrition (adjusted difference=2.9, CI95%=1.2-4.6, p=0.001), but not smoking. Among secondary outcomes, symptom scores on the Quick Inventory of Depressive Symptomatology (QIDS-SR) were lower at follow-up for HI (adjusted difference=4.9, p=0.006). Other outcomes did not differ. Nine (39%) LI and 12 (41%) HI participants completed the final follow-up. Conclusions: Personalized health coaching for youth with psychosis is feasible and may have sustained benefits. However, engagement and retention with this population for 12 weeks is challenging.
Integrated Care Conference | October 16th - 18th | Raleigh, North Carolina

Leave a Reply