Presenters
- Tyler Lawrence, PhD, Behavioral Health Faculty, Sea Mar Marysville Family Medicine Residency, Marysville, Washington
- Jennifer Caspari, PhD, Director of Behavioral Medicine, General Internal Medicine, University of Nebraska Medical Center, Omaha, Nebraska
- Elizabeth Lyden, MS, Associate Director, Center for Collaboration on Research, Design and Analysis, University of Nebraska Medical Center, Omaha, Nebraska
Summary
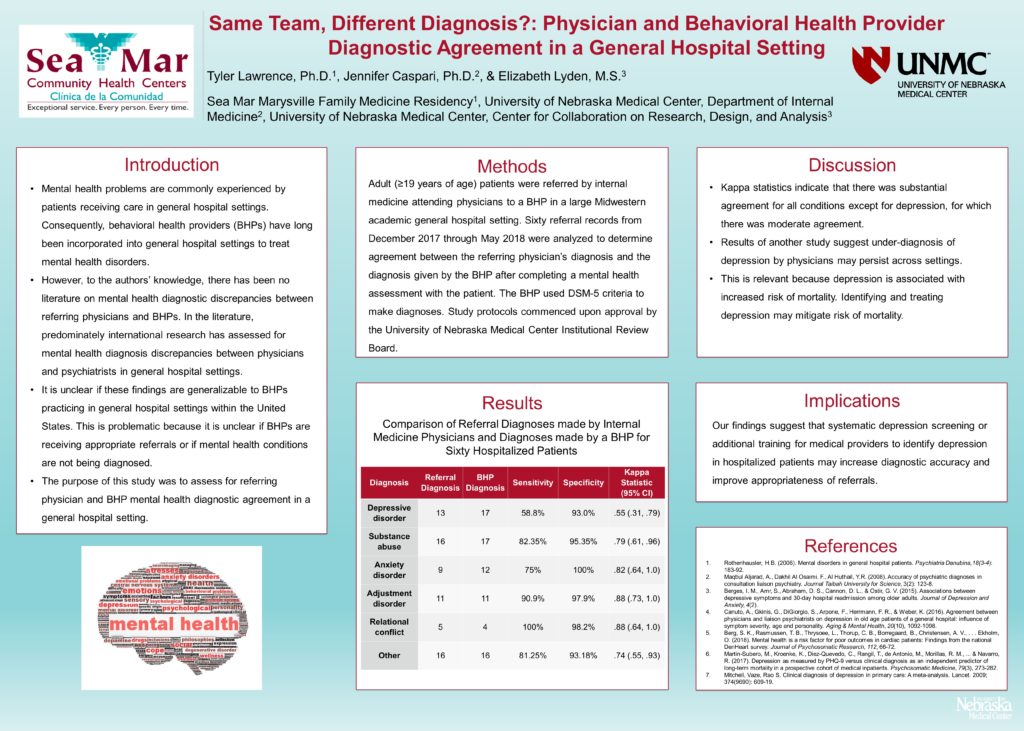
The integration of behavioral health providers (BHPs) in general hospital settings is potentially advantageous because hospitalized patients can have complex care needs and have high rates of psychosocial problems. Physicians are often the gatekeepers for identifying patients with psychosocial problems and referring them to a BHP. However, to our knowledge, there has been no literature on mental health diagnostic discrepancies between referring physicians and BHPs. Assessing for discrepancies between hospital physician and BHPs diagnosis may be beneficial for two main reasons. First, low diagnostic agreement would suggest behavioral health services are often used inappropriately. Second, it would highlight a potential need for systematic screening or training on psychosocial health screening in hospitals to identify patients with mental psychosocial problems. Attendees will learn about the results of study assessing for diagnostic agreement between initial physician diagnosis and BHPs’ diagnosis for 60 inpatient physician referrals. The sample consisted of an equal number of male and female patients. The majority of patients were white (73%), followed by African American (25%), and American Indian (1.7%). The mean sample age was 55.5 (SD=13.9) years old. Diagnostic agreement was assessed using the kappa statistic with a coefficient ≥0.7 being considered substantial agreement. Kappa statistics indicated good agreement between initial physician diagnoses and BHP diagnoses for substance abuse (.79), anxiety disorders (.82), adjustment disorders (.88), relational conflict (.88), and “other” (.74). There was lower agreement for depressive disorders (.55). While diagnostic agreement for many conditions was better than anticipated, there was lower diagnostic agreement for depression. This suggests systematic depression screening or training medical providers to identify depression in hospitalized patients may increase diagnostic accuracy and improve appropriateness of referral rates. Hospitalized patients frequently have very complex biopsychosocial-spiritual needs. Thus, the focus of this presentation is directly in line with the conference theme. Presentation content will be applicable to a wide audience; especially providers, physicians, and administrators whose roles include work in a hospital setting.
Objectives
- Describe the importance of integrating behavioral health providers into general hospital settings.
- Identify the psychosocial conditions that appear to be underdiagnosed in a general hospital setting.
- List the methods for improving the accuracy of diagnosing psychosocial conditions.

Leave a Reply