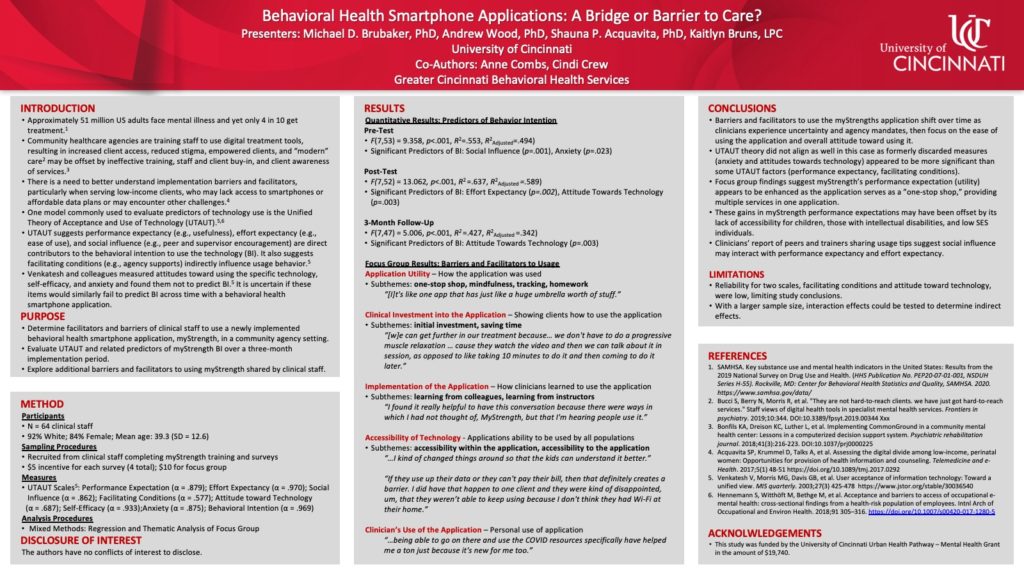
Approximately 51 million US adults face mental illness and yet only 4 in 10 get treatment. To be accessible and relevant across generations, community healthcare agencies are training new clinical staff to use digital treatment tools and create systems of care supporting their use. The benefits of increased access, reduced stigma, empowered clients, and “modern” care may be offset by ineffective training, staff and client buy-in, and client awareness of services. There is a need to better understand implementation barriers and facilitators, particularly when serving low-income clients, who may lack access to access to smartphones or affordable data plans or may encounter other challenges. Participants include a sample of 64 clinical staff, 92% White, 84% Female, mean age 39.3 years (SD = 12.6). This mixed methods implementation study, used multiple regression analyses to predict the behavioral intention (BI) to use an evidence-based mobile health app (myStrength) across four time points from pre-training to six-month follow up. Performance expectancy, effort expectancy, attitudes towards technology, social influence, facilitating conditions, self-efficacy, and anxiety were measured using the Unified Theory of Acceptance and Use of Technology, commonly used to assess e-health technologies. Focus group data was analyzed, revealing five themes: application utility, clinical investment, implementation processes, technology accessibility, and clinician’s use of the application. Regression analyses indicate the model explained 49%, 59%, and 34% of the BI variance at respective pre, post, and 3 month follow up (6 month data in process). Individual variables reaching statistical significance revealed a shift from social influence and anxiety (pre-training), to effort expectancy and attitudes towards technology (post-training), with only attitudes towards technology remaining at follow up. Results show training may facilitate usage; however some barriers persist.
Spring Virtual Conference April 17-18th | In-Person Annual Conference in San Antonio, TX Oct 24-26th

Leave a Reply