Presenters
- Lauren Dennelly, LCSW, Behavioral Health Specialist at Lehigh Valley Health Network and Doctoral Candidate; Bryn Mawr Graduate School of Social Work and Social Research, Bryn Mawr, PA
- Sara Bressi, PhD, LSW, Associate Professor of Social Work; Bryn Mawr Graduate School of Social Work and Social Research, Bryn Mawr, PA
Summary
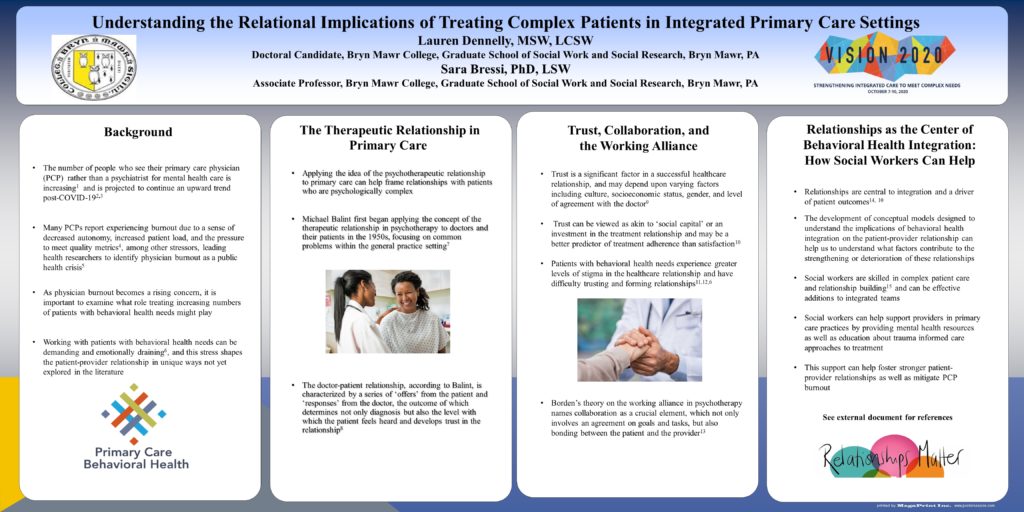
Primary care continues to be on the front lines of care in treating more socially and behaviorally complex patients. However, the ways in which the patient-physician relationship are shaped as a result of this increasing complexity in primary care are not clearly understood. In order to provide quality care that effectively addresses social and behavioral health needs and leads to positive patient outcomes, greater attention needs to be paid to the influence this care has on the patient-provider relationship. This presentation will outline a burgeoning conceptual model developed to understand the implications of treating behavioral health conditions in primary care on the patient-physician relationship. The model addresses issues of trust and collaboration in the context of the working alliance (Bordin,1979) as well as frames patient-physician interactions through the lens of the therapeutic relationship in psychotherapy (Balint, 2000). The presentation will also highlight the importance of interprofessional collaboration with social workers in helping to facilitate improved provider relationships with complex patients and as well as mitigating provider burnout.
Objectives
- Define the concept of the therapeutic relationship in psychotherapy as applied to the primary care relationship.
- Identify elements of trust and collaboration as related to the primary care working alliance and the importance of maintaining these elements in relationships with complex patients.
- Discuss the implications of treating increasing numbers of patients with complex social and behavioral health needs on the therapeutic relationship in primary care and physician burnout and identify potential solutions to mitigating provider burnout

Your poster makes a great point. So much of caring for complex patients is not only on building a relationship with them, but the provider learning to manage that relationship well, as in the psychotherapeutic relationship. It would be interesting if you could suggest some specific ways social workers can help providers learn these skills.
I apologize for my (very) late response to this comment. I think one of the most important ways social workers can help providers develop these skills is through case conferences and curbside consults in which the provider can be present in the room and learn by observation—being able to discuss a common patient and share our method of work, along with some psychoeducation about patient context issues that make relationships challenging (trauma, medical conditions, etc.) can be a really useful start.