Presenters
- Diane Ellis, MSN, RN, CCRN, Assistant Professor of the Practice, Villanova University, M. Louise Fitzpatrick College of Nursing, Villanova, PA
- Tara Reddy, Senior Nursing Student, Villanova University, M. Louise Fitzpatrick College of Nursing, Villanova, PA
Summary
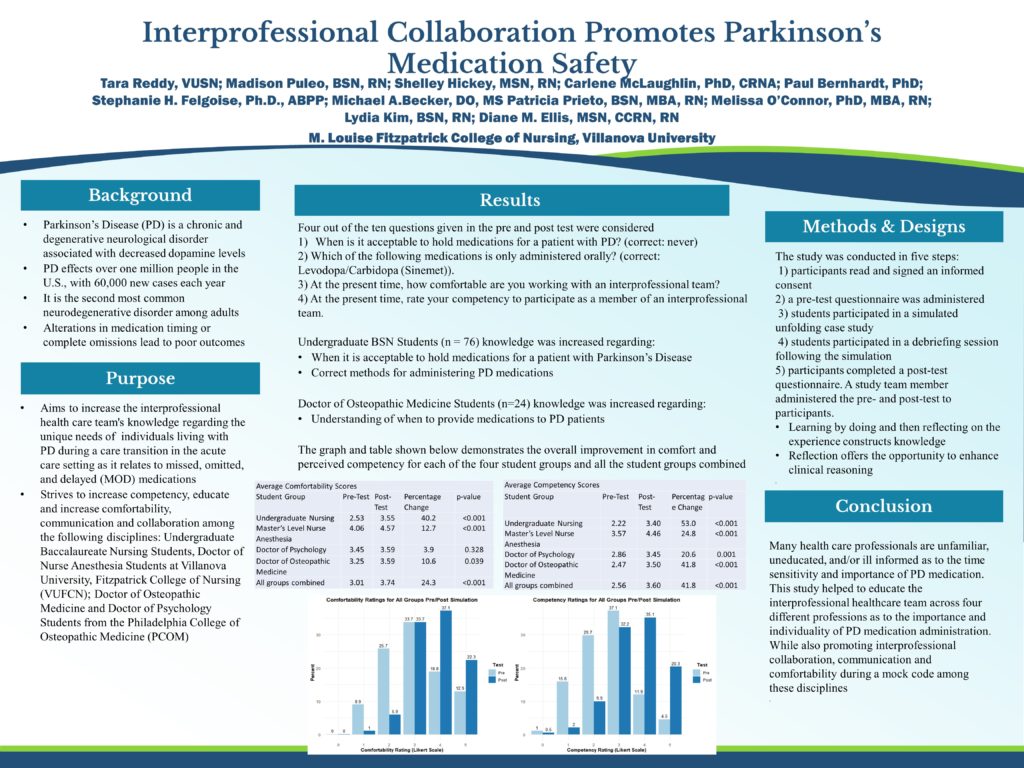
An Interprofessional Mock Code Care Transition-Parkinson’s Disease (PD) Patient Missed/Omitted/Delayed (MOD) Medication Simulation Case Study. This innovative and diverse simulation addressed a critical need to increase the competency among four healthcare professions to function during a mock code. While doing so, students gained requisite knowledge about Parkinson’s Disease, advanced directives, and roles and functions of this healthcare team. This interprofessional education initiative aimed to have students learn about, from, and with each other to enable effective communication and collaboration, and comfortability with unknown team members, which may ultimately lead to improved health outcomes (IPEC). An Interprofessional Mock Code Care Transition-Parkinson’s Disease (PD) Patient Missed/Omitted/Delayed (MOD) Medication Simulation Case Study. This innovative research study directly addresses a priority area to increase the competency of healthcare professionals on the care of people living with Parkinson’s Disease. This research has the potential to increase the interprofessional health care team’s knowledge regarding the unique needs of all individuals living with PD during a care transition in the acute care setting as it relates to their missed, omitted, and delayed (MOD) medications. The purpose of this study was to increase competency, educate and increase comfortability, communication, and collaboration among the following disciplines: Baccalaureate Degree Senior Nursing Students (n=76), Master’s and Doctoral Junior and Senior Nurse Anesthesia Students (n=24), Doctor of Osteopathic Medicine Fourth Year Students (n= 24), and Doctoral of Psychology Fourth Year Students (n=21). The required case-study simulation was of a patient’s care transition and ultimate code, with a family member present. Following the simulation, a process debriefing session was conducted by the PsyD students for the rest of the student healthcare team. The session concluded with an educational debriefing by nursing staff, with supplemental commentary provided by physician and psychology collaborating faculty. The aims of this simulation were: 1) Determine baseline understanding prior to the simulation of the four different groups of students regarding their comfort level and competency of working together during a mock code (valid-reliable pre-test), 2) Quantify the change in knowledge and perceived importance of competency and collaboration, following the mock code simulation and debriefing (valid-reliable post-test), 3) Determine the percent change in self-perceived competency, collaboration, communication, and comfortability following the mock code simulation and debriefing among the four professions (valid-reliable post-test). Combining the pre- and post- test data for all student types, statistically significant improvements were found for the following questions (each with p-value<0.001): • When is it acceptable to hold medications for a patient with Parkinson’s disease (PD)? (correct: Never) • Which of the following medications is only administered orally? (correct: Levodopa/Carbidopa (Sinemet)) • Which of the following equipment is required to prepare for an elective intubation? (correct: Providing a respiratory/intubation box at the bedside) The final two items asked students to evaluate their comfortability working with an interprofessional team and their competency working with an interprofessional team on a scale from 0 to 5, with 0/1 corresponding to minimal or no comfortability/competency and 2-5 corresponding to moderate to extreme comfortability. Among all students who reported minimal to no comfortability/competency before the mock code, 93.3% and 92.9%, respectively, reported at least moderate comfortability/competency in the post-test. Average raw scores increased most substantially for undergraduate students, from 2.32 and 2.04, respectively, to 3.47 and 3.33, respectively. This simulation educated interprofessional healthca
Objectives
- Determine baseline understanding prior to the simulation of the four different groups of students regarding their comfort level and competency of working together during a mock code
- Quantify the change in knowledge and perceived importance of competency and collaboration, following the mock code simulation and debriefing
- Determine the percent change in self-perceived competency, collaboration, communication, and comfortability following the mock code simulation and debriefing among the four professions

Leave a Reply