Presenters
- Emmy Stup, MPH, Director of Practice Transformation and Value Based Programs, Thomas Jefferson University, Philadelphia, PA
- Tanya Dougherty, PharmD, BCPS, Population Health Pharmacist, Jefferson Health, Philadelphia, PA
- Maya Yancy-Hunte, CCMA, Practice Transformation Coordinator, Thomas Jefferson University, Philadelphia, PA
- Rachelle Rene, PhD, BCB, HSMI, Director of Primary Care Integrated Behavioral Health, Thomas Jefferson University, Philadelphia, PA
- Lawrence Ward, MD, Executive Vice Chairman & Vice-Chair, Clinical Practice & Quality, Thomas Jefferson University, Philadelphia, PA
- Emily Scopelliti, PharmD, BCPS, Associate Professor of Pharmacy Practice at Thomas Jefferson University, Philadelphia, PA
- Bracken Babula, MD, Clinical Assistant Professor, Thomas Jefferson University, Philadelphia, PA
Summary
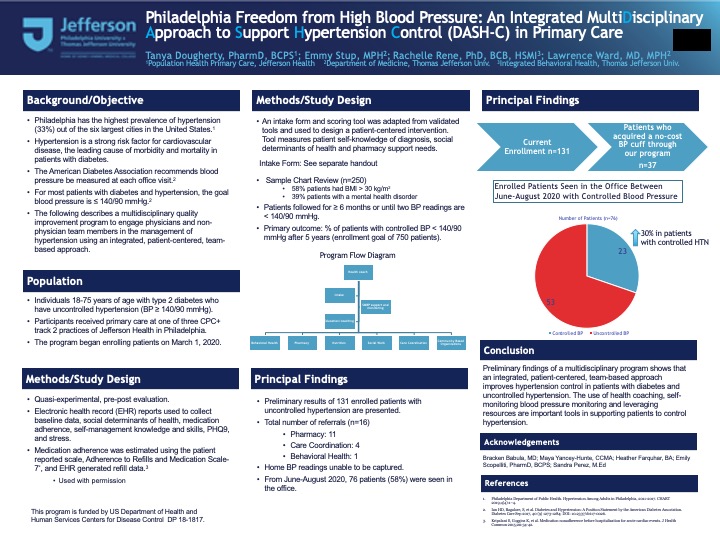
Philadelphia Freedom from High Blood Pressure: An Integrated MultiDisciplinary Approach to Support Hypertension Control (DASH-C) in Primary Care Rationale: Philadelphia has the highest prevalence of hypertension (33%) out of the six largest US cities. Population: This program is conducted in three CPC track 2 Primary Care practices of Jefferson Health in Philadelphia. Of patients 18-85 years of age with hypertension, 59% have controlled blood pressure (BP below 140/90). A sample chart review of 250 patients with hypertension shows that 58% have BMI over 30 and 39% have a mental health diagnosis indicating a complex patient population. Study design: Quasi-experimental, pre-post evaluation of an interdisciplinary quality improvement program on hypertension control using an integrated, patient-centered, team-based approach. Data Collection: EHR reports to collect: baseline data, social determinants, medication adherence (ARMS scale and refill data), self-management knowledge and skills, PHQ9, and stress. Procedures: Patient enrollment began 3/1/20 with a goal of 750 patients enrolled over 4 years. Based on an intake scoring tool, a patient-centered intervention will be designed with health coaching, home blood pressure monitoring, and referrals (behavioral health, pharmacy, nutrition, social work, care coordination, community organizations). Each professional assesses and manages patient specific factors with in-person or telephonic encounters until goals are achieved. Patients will be followed for at least 6 months or until two BP readings are below 140/90. All patients receive health coaching sessions and biweekly outreach and support. Results: The primary outcome of this program is the percent of patients with controlled BP below 140/90 after 4 years. Other outcomes: number of referrals, medication adherence, and patient related outcomes and satisfaction. Data will be analyzed using descriptive statistics and t-test for significance level. Results after 7 months of the program will be presented. Conclusions: Outcomes of a multidisciplinary integrated program within Primary Care on supporting hypertension control will be analyzed and presented.
Objectives
- List important elements in the implementation of a team-based approach to support uncontrolled hypertension.
- Identify unique skill set of each member in an interdisciplinary team, and how these skills complement each other.
- Identify patient-centered strategies to support patients with uncontrolled hypertension.

Leave a Reply